What is polycystic ovary syndrome (PCOS)?
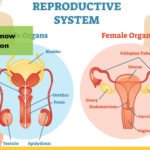
In a normal ovary, around five follicles (small sacs) develop each month, at the beginning of the menstrual cycle. These follicles contain eggs. Usually one follicle each month continues to develop until it releases an egg into the fallopian tube. This is known as ovulation. If the egg is fertilised by sperm, it travels down to the uterus, implants in the lining and a pregnancy begins. If the egg is not fertilised, the lining of the uterus is shed at the end of the monthly cycle and you have your period.
Polycystic ovaries have at least twice as many developing follicles as normal ovaries. However, many of these follicles do not mature to the point of releasing an egg (ovulation). Because they have more follicles than is usual, polycystic ovaries are slightly larger than normal ovaries.
Women with polycystic ovary syndrome (PCOS) rarely have all of the possible signs and symptoms described below. PCOS is therefore difficult to diagnose. The doctor will take account of your symptoms and will usually check your hormone levels (through a blood test) and your ovaries (through an ultrasound scan). PCOS runs in families.
What could PCOS mean for me?
If you have polycystic ovary syndrome (PCOS), you may become aware of some or all of the following symptoms. You may:
- Have more body hair than is usual for you
- Have irregular periods or no periods at all
- Have difficulty in getting pregnant
- Be overweight
- Have acne.
- These symptoms can vary from mild to severe. They can be caused by other conditions, too. If you have PCOS symptoms, you have a greater risk of developing long-term health problems such as:
- Heart problems
- Diabetes
- High blood pressure
- Cancer of the lining of the uterus (known as endometrial cancer).
What can help reduce long-term health risks?
Following a balanced diet and taking regular, appropriate exercise are the main ways in which you can help yourself. They can help reduce the long-term health risks associated with PCOS. If you are overweight, losing weight will help you. If your periods are irregular or non-existent they may become more normal. Follow advice from your doctor on reducing your calorie intake and taking more exercise. Increasing your activity is important step in any weight reduction program. Choose an aerobic activity such as walking or swimming, and start out slowly. You’ll find that with time you can increase your speed and distance and that the activity improves your state of mind as well as aiding in weight reduction.
Even if you are not overweight, you should take care to keep your weight within the normal range for your height.
Drugs known as ‘Insulin sensitizing agents’ (such as metformin) act by making the body more sensitive to insulin. These drugs can be used to help non-diabetic women who have PCOS.
Metformin reduces circulating insulin and androgen levels and restores normal ovulation in some women with PCOS. Even if metformin alone does not restore ovulation, it may improve a woman’s response to fertility drugs. Gastrointestinal irritation, especially diarrhea, is a common side effect.
Ovulation Induction
For women with PCOS who have difficulty in getting pregnant, induction of ovulation may be performed using either a five-day course of clomiphene citrate or a series of daily injections of another medication called human menopausal gonadotropin (hMG) or follicle stimulating hormone (FSH).
The decision of which medication to use is based on your individual needs and how you respond to therapy. You and your physician should discuss your options and decide which one is best for you.
Surgery
In very rare cases, ovulation is not achieved with clomiphene or hMG. If this happens, ovarian surgery may be needed to stimulate ovulation. This surgery can often be performed through the laparoscope using a laser or electrocautery instrument.